Individual Projects
Emergences of palliative care in paediatrics
Paediatric palliative care has crystallized into a distinct set of ideals and practices over the past decade. It is an active and total approach that focuses on the improvement of quality of life and the prevention and relief of suffering of children with life-limiting or -threatening conditions, and the provision of support for their family.
However, despite the growing institutionalization of paediatric palliative care in the form of paediatric palliative care teams, many children with serious diseases and their families are never offered the option to receive treatment and care that reliefs their suffering and improves their quality of life. If they do, this happens often late in the illness trajectory.
Against this backdrop, this project asks how paediatric palliative care teams becomes involved in the provision of treatment and care of individual patients. Further, it investigates the ways that infrastructures are developed for the provision of such services behind the scenes.
Drawing on ethnographic fieldwork carried out in a Swiss hospital and qualitative interviews with Swiss pediatricians particularly engaged around the issue, the project sheds light on the ways in which how paediatricians come to (not) involve their colleagues from the paediatric palliative care team; and how clinicians mobilise for the development of healthcare services in Switzerland. By doing so, the project contributes to current debates on “good care”, asymmetries and power, critique of medicine, health activism, and emotions in research.
Grid containing content elements
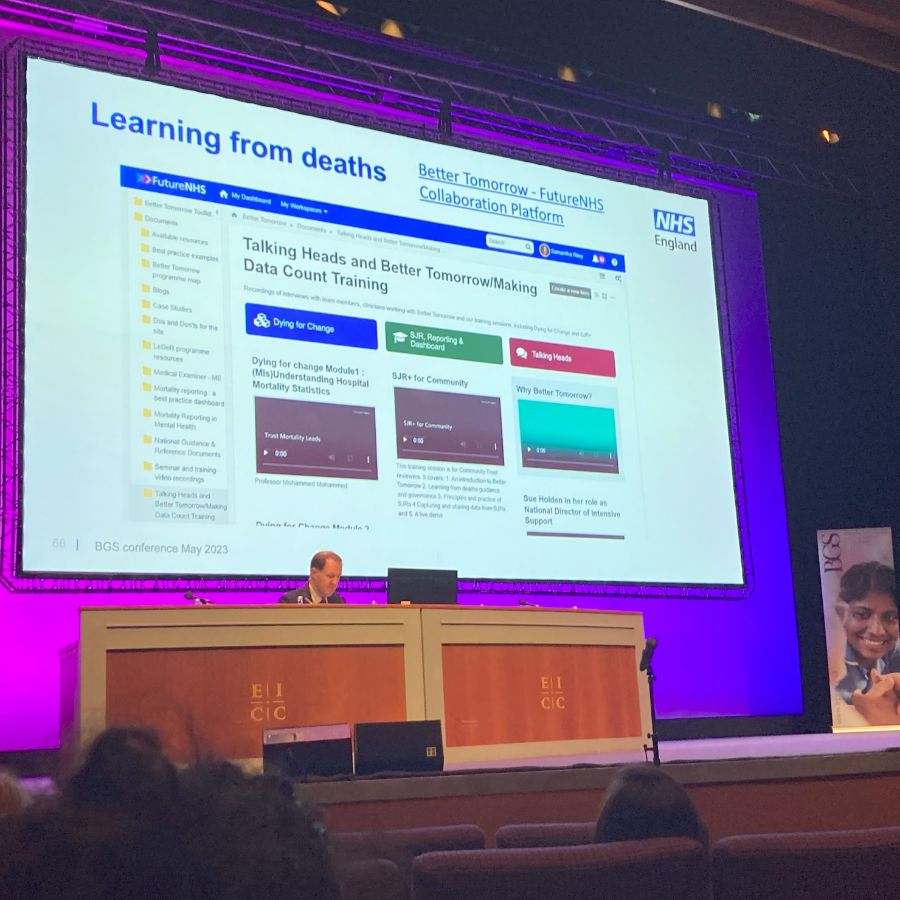
Careful limits amid uncertain endings in geriatric medicine
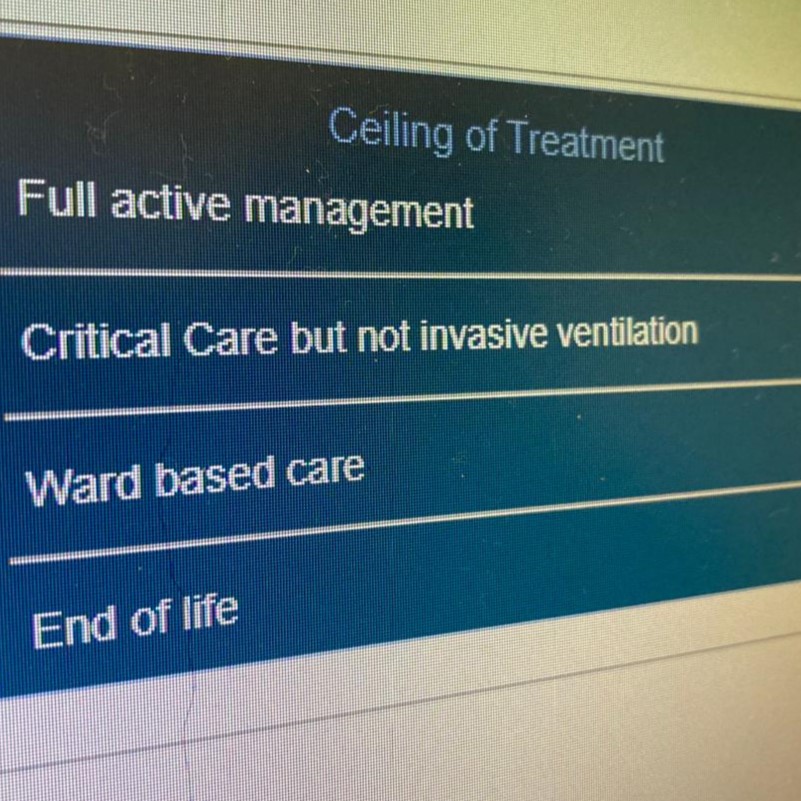
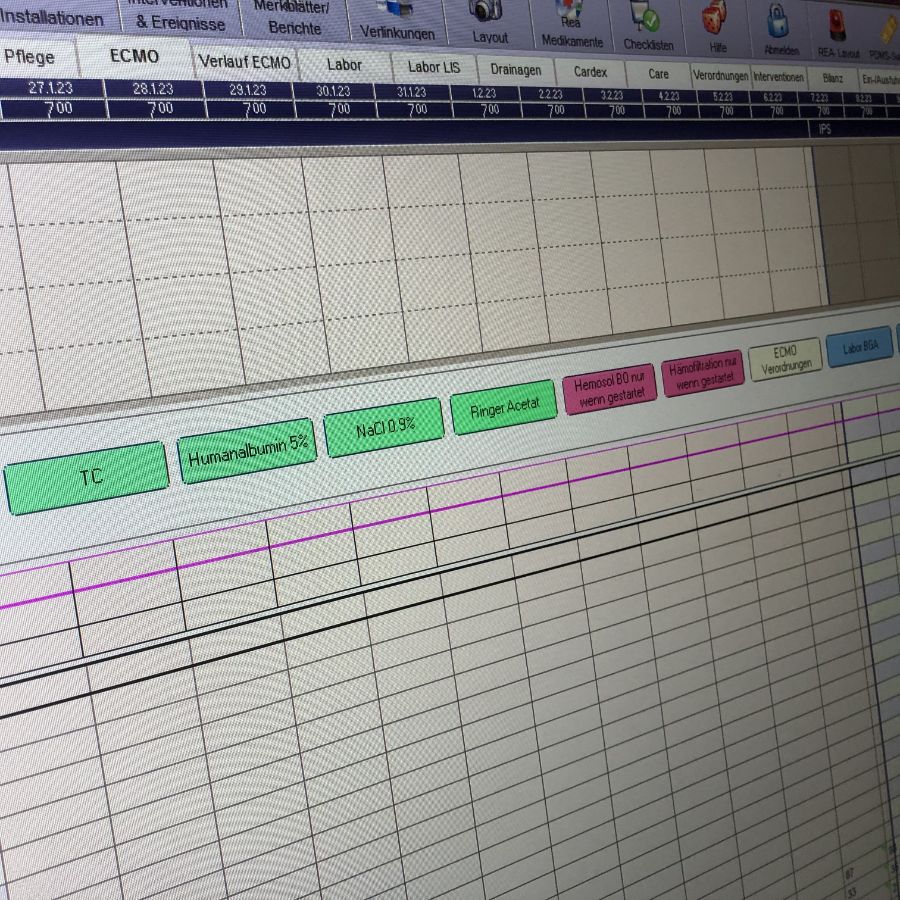
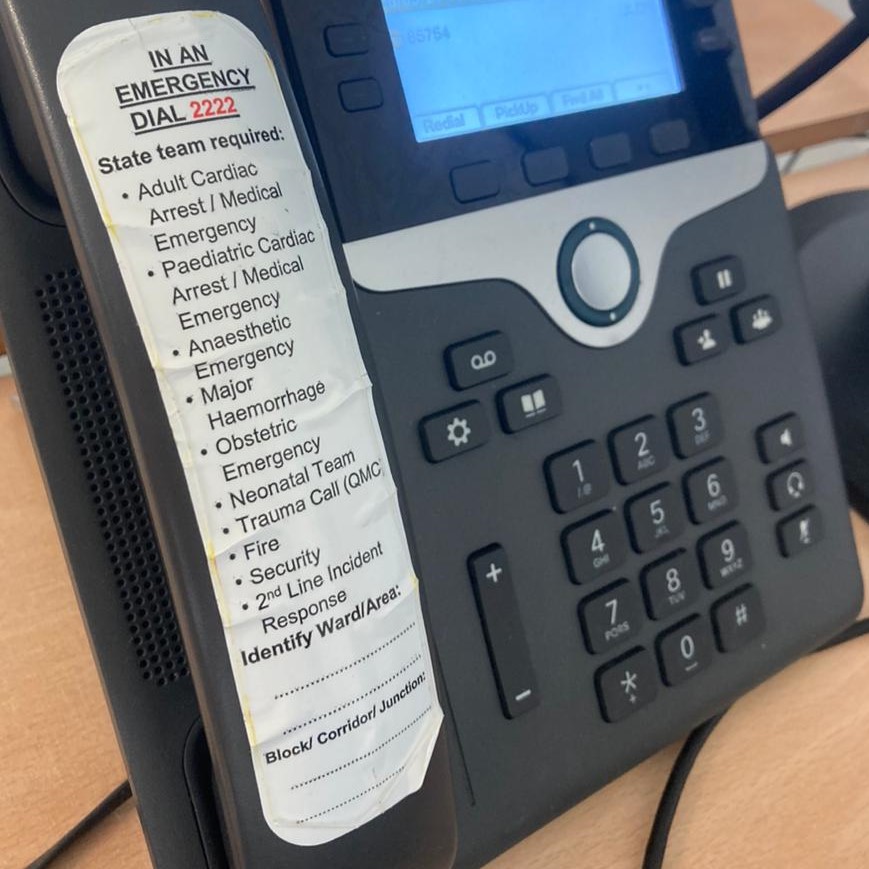
In the United Kingdom, older adults approaching the end of life are routinely admitted to hospital. Here, they are cared for by a number of healthcare professionals including specialists geriatricians. Geriatricians practice a generalist medicine that specializes in the care of older adults who come to hospital. Such patients present with abrupt or acute deteriorations of health or function, against a backdrop of clinical frailty and complex co-morbidity.
Geriatricians work with multidisciplinary teams to an ideal of holism and person-centred care, combining and balancing the practices and ideals of acute, rehabilitative, supportive and palliative care for patients with an uncertain illness trajectory. At the front line of care, such healthcare professionals and their colleagues work within a context of clinical uncertainty. Statistically, half of the patients they care for will die within a year of admission.
This project asks how within this uncertainty, specialists in geriatric medicine strive to deliver good care to patients who may, or may not be, approaching the very end of their life. It does so with an eye to how such care is delivered in practice, alongside ideals, technologies, vulnerable bodies and the careful limits this care involves.
Drawing on ethnographic fieldwork in three hospitals in the UK and qualitative interviews with multidisciplinary healthcare professionals, this project elaborates the nature and logics of non-life prolonging forms of care in geriatric medicine and it's mediation by digital care platforms. By doing so, the project contributes to current debates on "good care", valuation, technologies, critique of medicine, and absence.





.jpg 900h)
.jpg 900h)